Dr. Rafael Grossmann Test Drives the First Cloud Gaming Platform in Healthcare
We’re always working to improve our games and tools for doctors and other medical professionals.
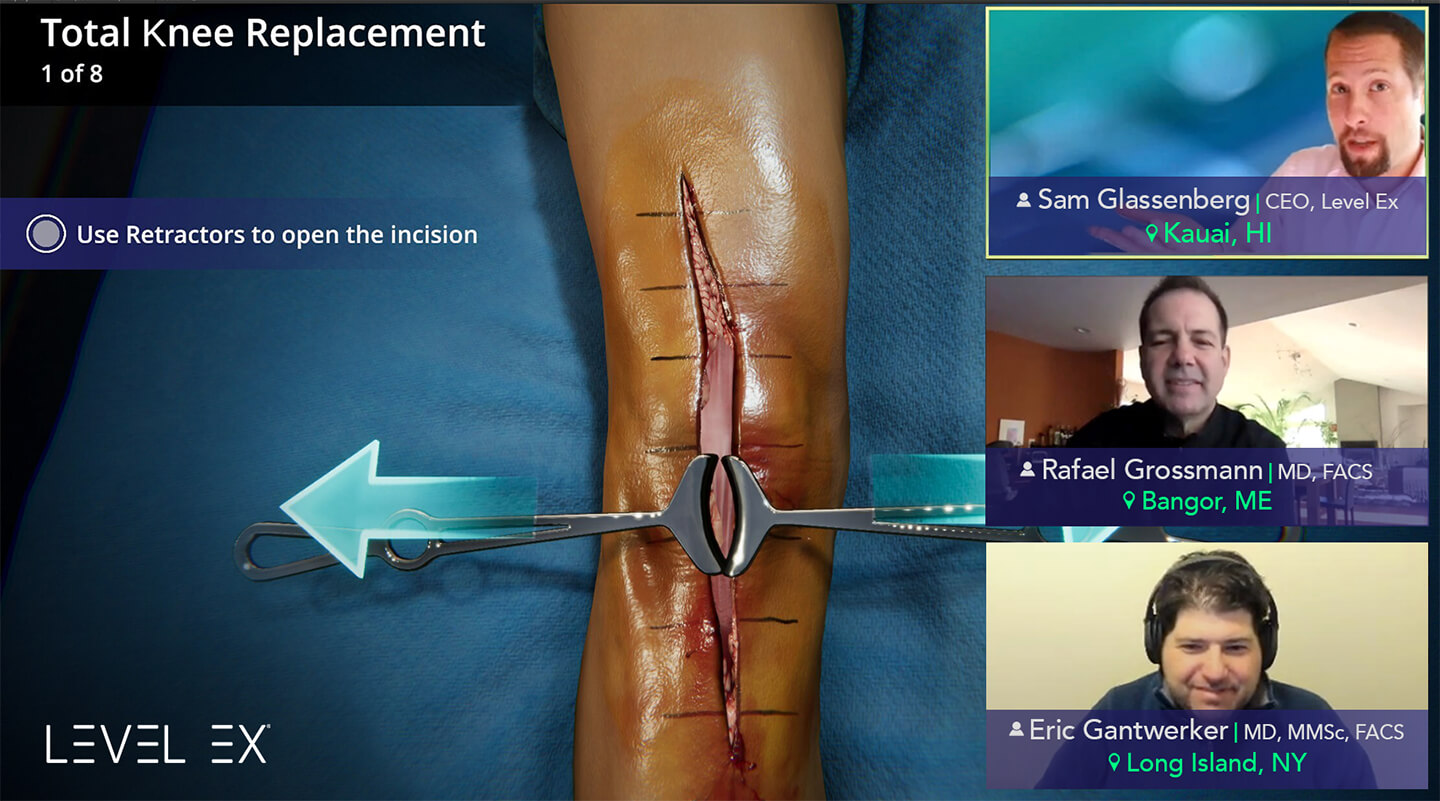
Most recently, our team created the first cloud gaming platform in healthcare—a powerful way for doctors to remotely collaborate and work together on diagnosing and treating virtual patients in real time—and we’re excited to show it off to the medical community.
So we sat down for an online session with Dr. Rafael Grossmann, a world renowned trauma surgeon, medical futurist, and respected authority on tech innovation in healthcare. Our three participants were separated by thousands of miles (and even some ocean) as we explored virtual surgery and COVID-19 virtual patient cases together. See the highlights of that session in this short video:
Watch the Full Discussion
Read the Transcript Below
Level Ex Team: At Level Ex we’re a team made up of video game designers, artists, doctors, and medical professionals, all working together to capture the practice of medicine as video games. So we sat down with Dr. Rafael Grossmann, a world renowned trauma surgeon and medical futurist, whose opinion is highly sought after on the medical applications of new technologies. Our team has built the first cloud gaming platform in healthcare, and we were eager to get Dr. Grossmann’s perspective as three people in completely different parts of the country collaborate on giving medical care to virtual patients.
Sam Glassenberg [00:34]: I’m doing this here on my computer. Now I’m going to put my hands up. You open up the patient on the right. Let’s talk about what’s happening here. You and I are thousands of miles apart, and yet here we’re doing virtual surgery on a patient that’s simulated in the cloud. I’ll go ahead and bend the knee into position. Now you’ll notice you didn’t have to install anything. You just got a QR code, tapped a link, pressed play, and next thing you know, we’re doing virtual surgery together.
I, as the host, I’m in control of the camera. I can show you this knee from any angle; I can place the cut guide. Then we can show the angle relative to the femur. I can insert it to depth. Here I’ll adjust the cut guide rotation. All you have to do is click or tap on the dial and then move it to the red wedge. I’ll insert it to depth—so you and I are doing surgery together on a virtual patient. You don’t have to install anything. I think you’re probably seeing it’s pretty responsive for you.
Level Ex Team [01:47]: In addition to virtual surgery, we’ve also been working to find ways of collaborating on virtual patient cases so that doctors can discuss and internalize best practices for diagnosing and managing challenging case scenarios. Next, we had Dr. Grossmann and Dr. Eric Gantwerker, a pediatric otolaryngologist and Level Ex’s medical director, work together to secure the airways of multiple virtual patients who may have COVID-19.
Dr. Eric Gantwerker [02:14]: This is a really difficult patient. This is a 36 year old male who is COVID-19 positive, who had a motor vehicle collision, and currently has an uncleared C spine and a GCS of seven.
Dr. Rafael Grossmann [02:26]: We have no idea about the COVID-19 risk, so we’re going to don and get ready. Then we’re going to limit the standing room as we should always do. We’re going to preoxygenate this patient. This is a bit more tricky because this patient has a full stomach and has a head injury. I would say you preoxygenate. Traditionally we would do non-rebreather. I’m going to go the way of the non-rebreather, but this is a patient that has a full stomach, so this is risky to do.
Sam Glassenberg [03:00]: Dr. Gantwerker, do you want to recommend the next step?
Dr. Eric Gantwerker [03:02]: I was going to say, this is a tough situation because as an otolaryngologist and airway person, paralyzing somebody who you’re not sure you’re going to be able to intubate is very anxiety provoking for me. I know the COVID-19 recommendations are to do an RSI or rapid sequence intubation, but I would consult my trauma surgeon Dr. Grossmann to find out what he would recommend.
Dr. Rafael Grossmann [03:30]: A rapid sequence is probably the right thing to do. In a trauma patient, you’re thinking about a spine immobilization, which makes things more difficult. But you do have a low saturation, so you’ve got to bring that up. It went up as we can see on the right side to 96%, so we do have some time. We don’t really know that he has a full stomach, but he probably does. We kind of assume that all the time. Doing a rapid sequence would be the way to go, especially when you have a trauma surgeon in the room and always the option for a surgical airway.
Dr. Eric Gantwerker [04:17]: Absolutely.
Dr. Rafael Grossmann [04:18]: If you need to, you go that route.
Dr. Eric Gantwerker [04:22]: All right, so we’re going to do RSI.
Sam Glassenberg [04:24]: We’re all interacting with it. Go ahead. There we go.
Dr. Eric Gantwerker [04:26]: Perfect, the patient’s asleep and paralyzed. Whew. All right.
Sam Glassenberg [04:32]: Dr. Gantwerker, do you want to call for assistance?
Dr. Eric Gantwerker [04:36]: That’s a really good idea. We should definitely call for an airway expert in the room. We also have our trauma surgeon who also is our airway expert, so I think we’re in a good place. We’ve definitely loaded the boat. We’re at the point now where we should probably intubate. You can see already that the patient desaturated 92%, which we know in the COVID-19 positive patient population that they actually drop very quickly upon induction. This is definitely something that we need to consider as we progress through this case, so in this particular case, what do you think, Dr. Grossmann?
Dr. Rafael Grossmann [05:18]: I stay away from this patient’s face, given the risk, so I think a video laryngoscope would be the way to go, and you always have a bougie ready. It gives you something you go through, and then you intubate over that.
Dr. Eric Gantwerker [05:33]: Absolutely.
Dr. Eric Gantwerker [05:33]: Perfect. Let’s do that. Oof.
Sam Glassenberg [05:39]: You can see that the airway is filled with blood.
Dr. Eric Gantwerker [05:44]: That’s not something we wanted.
Sam Glassenberg [05:47]: This is going to get interesting.
Dr. Rafael Grossmann [05:48]: That’s all right because we didn’t have the option to aspirate. You always have to look at the airway, the oropharynx. You’ve got suction and have everything that you need to ready.
Sam Glassenberg [06:01]: Let’s do suction.
Dr. Eric Gantwerker [06:02]: Yeah, let’s do that. That’s a good idea. Oof.
Dr. Rafael Grossmann [06:07]: You have 83% saturation. You already called for assistance—I don’t know what type of assistance, but I’m going to hit more options to see because again this is a patient who is now with an airway, or oral pharynx, which is blocked in a way visually for safe intubation and is already hypoxic. You are getting pretty close to having to jump in and do a surgical airway like a cricothyrotomy, so let’s see what this is showing here. I’m going to hit prep surgical.
Sam Glassenberg [06:41]: Go for it.
Dr. Eric Gantwerker [06:43]: That’s where I would agree.
Dr. Rafael Grossmann [06:44]: So we’re back to, well, so we’re now at 78, and so—
Dr. Eric Gantwerker [06:49]: My heart is pounding.
Dr. Rafael Grossmann [06:52]: To tell you the truth, with a 78% saturation, and you have an oral pharynx full of blood, I think that it depends on who is in the room. If you attempt intubation, you might choose that, but you don’t want to waste more than 15 seconds on that and then go to a surgical airway.
Dr. Eric Gantwerker [07:10]: Absolutely.
Dr. Rafael Grossmann [07:11]: I hit this to see what happens, and we can’t use a bougie unless you really are seeing. We already tried all these other three options, and the pharynx is full of blood. I’m going to go back and I’m going to see if I get the option to just go ahead and see what the surgical airway.
Sam Glassenberg [07:32]: There you go.
Dr. Rafael Grossmann [07:34]: Emergency invasive—that would mean a surgical airway?
Sam Glassenberg & Dr. Eric Gantwerker [07:37]: Yep.
Dr. Rafael Grossmann [07:39]: Big knife.
Sam Glassenberg [07:40]: Oh boy.
Dr. Rafael Grossmann [07:41]: 20 [hero points]!
Dr. Eric Gantwerker [07:41]: All right.
Sam Glassenberg [07:44]: What are your thoughts? Where should we be applying this? What are the opportunities?
Dr. Rafael Grossmann [07:49]: Like I always say, healthcare improvement is about improvement of communication and connectivity. Right now, we’re doing this virtually. We’re doing this with no boundaries. It happens instantaneously. It happens collaboratively. Healthcare is about teamwork. The beauty of this is that we are on a laptop computer. With a regular smartphone over connectivity, we can do very instructive and educational team building and skill building, lifesaving training.
Level Ex Team [08:29]: As Dr. Grossmann said, the improvement of the medical system is about advancing communication, connectivity, collaboration, and teamwork—and discovering creative ways to solve these problems is what drives us. You can learn more about us at levelex.com and don’t forget to follow Dr. Grossmann at rafaelgrossmann.com. From Level Ex, thanks for watching.
Learn more about Dr. Grossmann at his website: rafaelgrossmann.com