Dr. Peter Lio, renowned dermatologist and physician advisor, and Dr. Eric Gantwerker, Vice President, Medical Director for Level Ex, discuss our new dermatology game, Top Derm, on the Dermasphere podcast. Co-hosts Dr. Michelle Tarbox and Dr. Luke Johnson ask them about the game development process, dermatology trends, and the future of the field as the hosts share their reactions to playing the game.
“One thing that I loved about [Top Derm] is that it lets you make decisions… These are the decisions we make all day in clinic… It lets you practice that decision tree and then gives you feedback immediately after, which is one of the most powerful ways to learn.”
—Michelle Tarbox, MD, Co-host of the Dermasphere podcast, Assistant Professor of Dermatology at Texas Tech University Health Sciences Center
Listen to the Episode
Contributors
Michelle Tarbox, MD
Co-host of the Dermasphere Podcast, Assistant Professor of Dermatology at Texas Tech University Health Sciences Center, fellowship-trained in dermatopathology
Luke Johnson, MD
Co-host of the Dermasphere Podcast, Assistant Professor of Dermatology at the University of Utah School of Medicine, fellowship-trained in pediatric dermatology
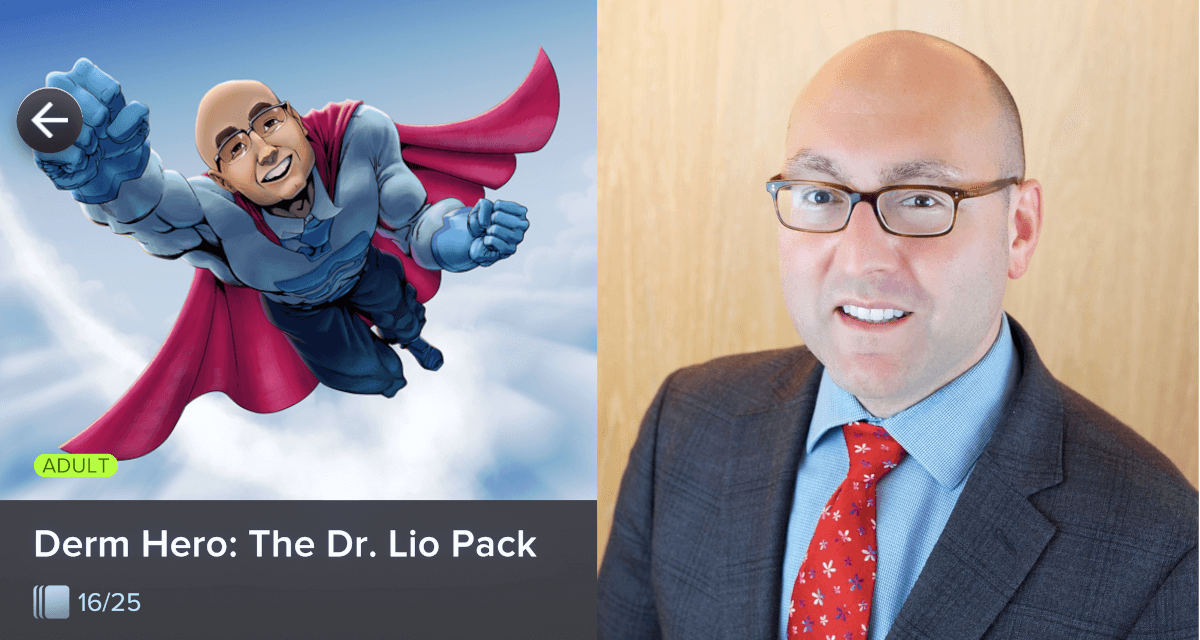
Peter Lio, MD, FAAD
Medical Dermatology Associates of Chicago, Clinical Assistant Professor of Dermatology & Pediatrics at Northwestern University Feinberg School of Medicine, atopic dermatitis expert, Lead Physician Advisor for *Top Derm*
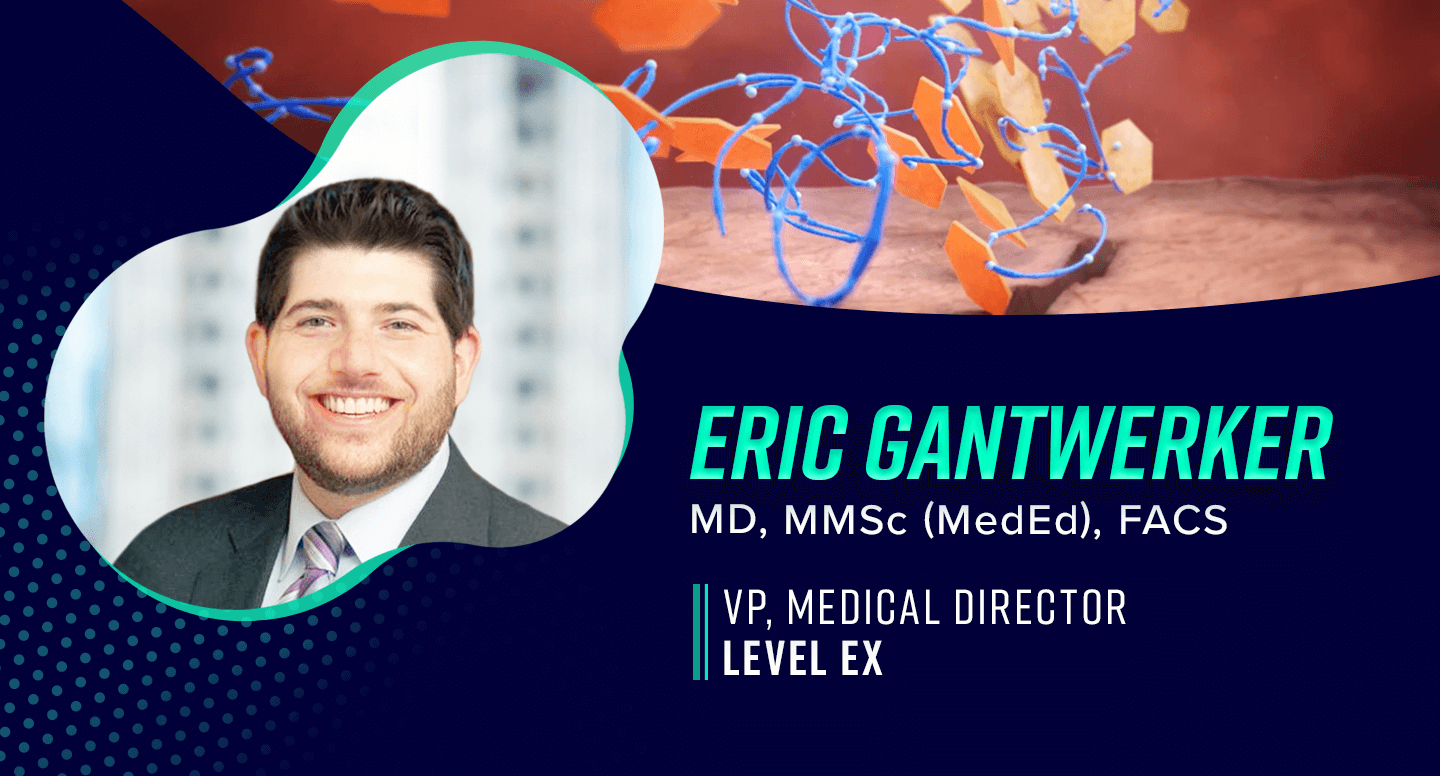
Eric Gantwerker, MD, MMSC (MEDED), FACS
Vice President, Medical Director at Level Ex, Pediatric Otolaryngologist at Cohen Children’s Hospital Northwell Health/Hofstra, Holds a MMSc in Medical Education from Harvard Medical School and an MS in Physiology and Biophysics from Georgetown University
Read the Transcript Below
Dr. Johnson: Hello, friends and colleagues, and welcome to Dermasphere, the podcast by dermatologists for dermatologists and for the dermatologically curious. I’m one of your hosts. My name is Luke Johnson. I’m a pediatric dermatologist and general dermatologist with the University of Utah. And my co-host, of course, is—
Dr. Tarbox: This is Michelle Tarbox. I am an Associate Professor of Dermatology and Dermatopathology at Texas Tech University Health Sciences Center in beautiful, sunny Lubbock, Texas.
Dr. Johnson: This is a bonus episode of Dermasphere. Normally we come to your ears every two weeks with discussions with some of the latest, and we like to think, most relevant research in the world of clinical dermatology. Today we’re going to do something a bit different. We’re going to discuss not an article and not an area of research, but a new dermatology app that is available. It’s called Top Derm and get ready for this: It is a dermatology game published by a studio called Level Ex. To help us discuss it, we have two members of the Level Ex team here with us today, Dr. Gantwerker and Dr. Lio, thanks so much for joining us. Do you want to start by introducing yourselves?
Dr. Lio: Wonderful. Thank you so much for having us. My name is Peter Lio. I’m a clinical Assistant Professor of Dermatology and Pediatrics at Northwestern University in Chicago. I am excited to be in the position of lead advisor for the Top Derm game. I’m the dermatology representative among a group of dermatologists who have helped put together the game.
Dr. Gantwerker: Thank you so much for having me. I’m a pediatric otolaryngologist, Dr. Eric Gantwerker, and I’m not a dermatologist, so I apologize. But I also wear a hat. I’m in academic practice in New York at a tertiary care center and Associate Professor of Otolaryngology and the Vice President, Medical Director of Level Ex. I started as an advisor and now oversee everything from a strategy, education, and medical standpoint. I have a master’s in medical education, which is my background.
Dr. Johnson: Super excited to have you here today to discuss this. By way of full disclosure, this episode does represent a partnership between Dermasphere and Level Ex. No money changed hands, listeners, but Level Ex did put out some advertising for this episode. Maybe you guys saw it. We thought that a collaboration between Dermasphere and Level Ex would be great for a lot of reasons. One, it allows us to get Peter Lio back on the show. He did join us in episode 47 to discuss topical steroid withdrawal syndrome. Also, I feel that Level Ex’s, especially this Top Derm game, and Dermasphere’s missions are really aligned. We all are trying to get people better at dermatology using various forms of technology that are out right now—podcasting and apps, etc. By the way, I should say that the Top Derm app is free, and also I love dermatology and I love games, and this is a dermatology game! Finally, peanut butter, meet chocolate! Dr. Lio, Dr. Gantwerker, I’d love to hear a summary of the game. We’ll start with that. Tell us about it.
Dr. Gantwerker: Dr. Lio, take it away, you’re integrally involved, so—
Dr. Lio: I will tell you a little bit from my perspective. One of the exciting things about Level Ex and this project is that it is something that continues to evolve and develop. I am hopeful that what we have today is going to be pretty different than what we have in a couple of years—that we’re going to be adding and developing and continuing to explore what we can do with this medium.
The basic impetus for the vision, Luke, is just like you: I love dermatology, I love games, and I love learning. What an amazing way to take some of the addictive quality of mobile games, which we know can work against us sometimes. You’re sitting there and you find yourself 20, 30 minutes have passed while you’re playing with some kind of coin game or jewel game, and you go, “Boy, I didn’t really get anything out of that.” What if we could leverage that to do some educational things, to practice some of the things that many of us already know—or we’re supposed to know when we studied for our boards—but we can review them?
For me, the part that’s particularly interesting is that, very much like the Dermasphere podcast, there are certain things you can do very well in a lecture. At a lecture, you can show certain slides; you can take an audience through a certain set of principles and instructions. Then there’s a lot you can’t do. So on a long form podcast like this, I love it because I love listening to you guys not only tell me about the article. That’s awesome. That by itself is worth the price of admission. I love when you guys digest it, discuss it, think about it, and put it to use because that’s what I remember when I’m actually in a clinic. I’m like, “Oh, yes. Michelle said this is how she likes to use this, or this is what she thought of it.” That extra bit of editorial, obviously very sophisticated editorial, helps me put it in place.
There are even additional things we can do in the context of a game. Within a game, we can now create scenarios to challenge you. We can present experiences where you might try something and then go, “Whoa, I don’t like what happened there.” Go back and try something different and then learn from those experiences—both the good and the bad. So from a general standpoint, I love this idea. We know that the secret of learning is repetition, and nothing lets us do more repetition than in a game. Then those subtle changes that we’re able to show you in a game—I mean, I could go on for a while and I’ll shut up in just a moment.
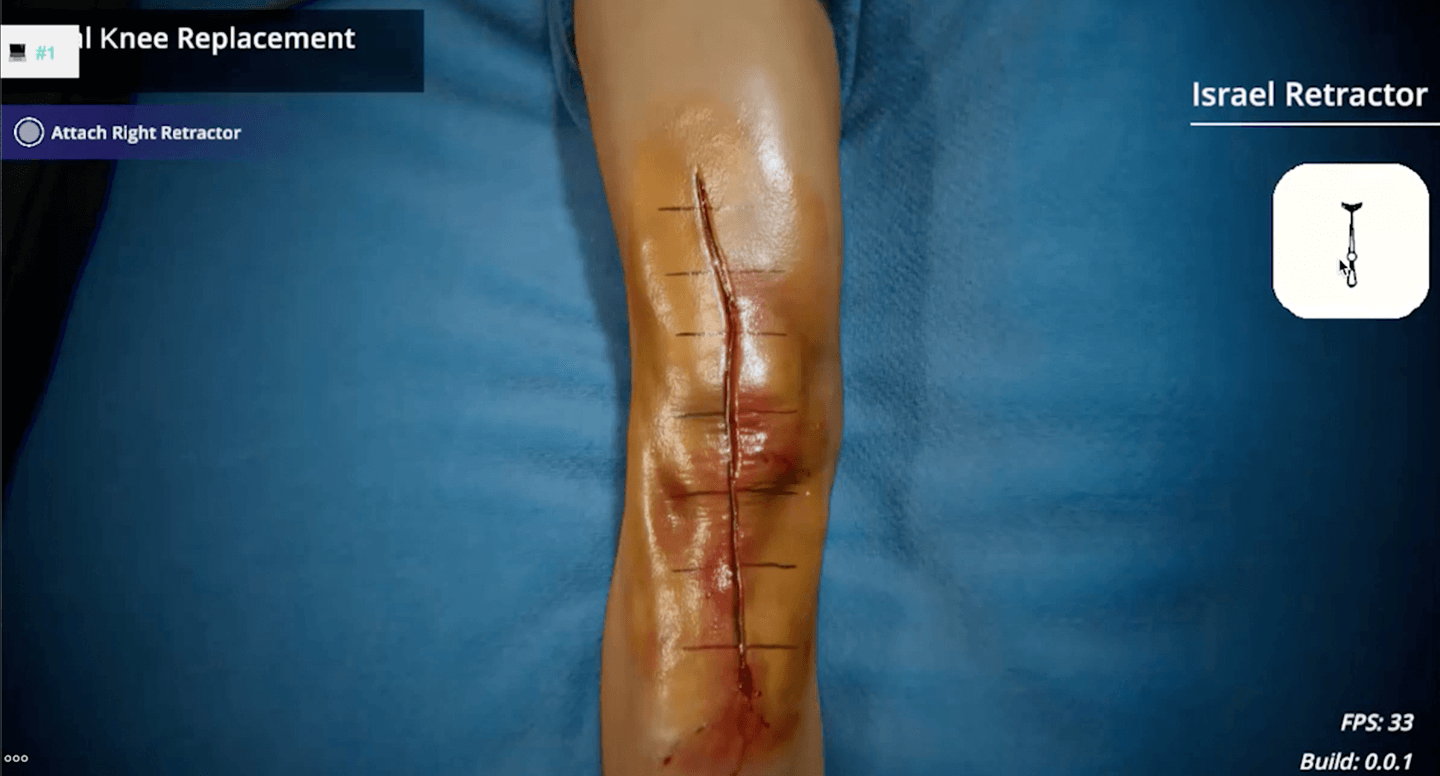
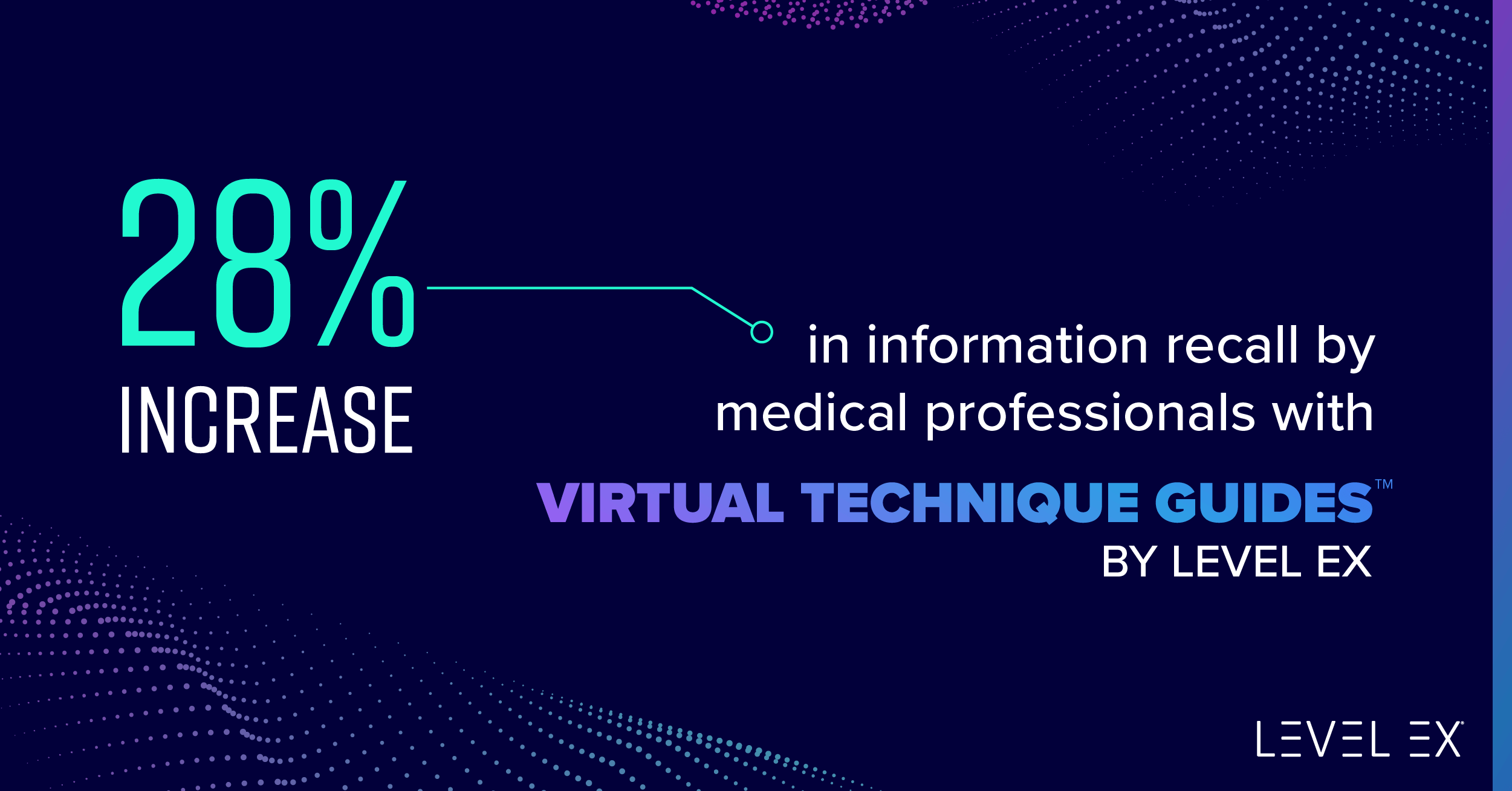
They have the most incredible art team doing specific renders of skin disease. We have lots of great photo atlases. We’re blessed that dermatology is very visual, but here we have a team of artists who can then tweak those images. They can enhance those images. The word I like to use—I don’t think the artists talk about it this way, but I love saying it—it’s hyper-real. You look at it, and it feels like that 8K image where everything’s crystal clear and they’re showing you the key pieces that we want you to see and minimizing some of the other pieces. It also allows us to show it in different skin types. You can show it across different skin tones, on more richly pigmented skin. You can see things that maybe you don’t get to see normally because you can render it. Then finally, it lets you play with some of the other aspects of disease: the type, the shape, the arrangement in the distribution, where maybe every photograph that you’ve ever seen is always on the back of somebody’s hand. That’s the most commonplace. Now we can move it to a different location to challenge our learners to think about it in a different way. So for all of these reasons, I think this is in some ways the future of education. It allows us to take a deep dive into how people learn and to reinforce strategies, but also to create novel and exciting clinical scenarios to challenge people.
Dr. Tarbox: That’s awesome. One thing that I loved about it is it lets you make decisions. That’s what we do in clinic all day long. I have never used Tinder because I’ve been married to Mr. Dr. Tarbox for a very long time, but I understand that there’s a lot of swiping right or left or something like that. Some of the game is a binary choice: infectious or noninfectious. These are the decisions we make all day in clinic. I’m looking at this rash: “Is it going to get better with antibiotics? Do I need an anti-inflammatory?” It lets you practice that decision tree and then gives you feedback immediately after, which is one of the most powerful ways to learn. I always tell my residents, if you commit to an answer and you’re right, you’ll get a little shot of serotonin. You’re going to remember it pretty well. If you commit to an answer and you’re wrong, it’s like “Not again, Satan,” and you will remember it forever.
Dr. Lio: Exactly.
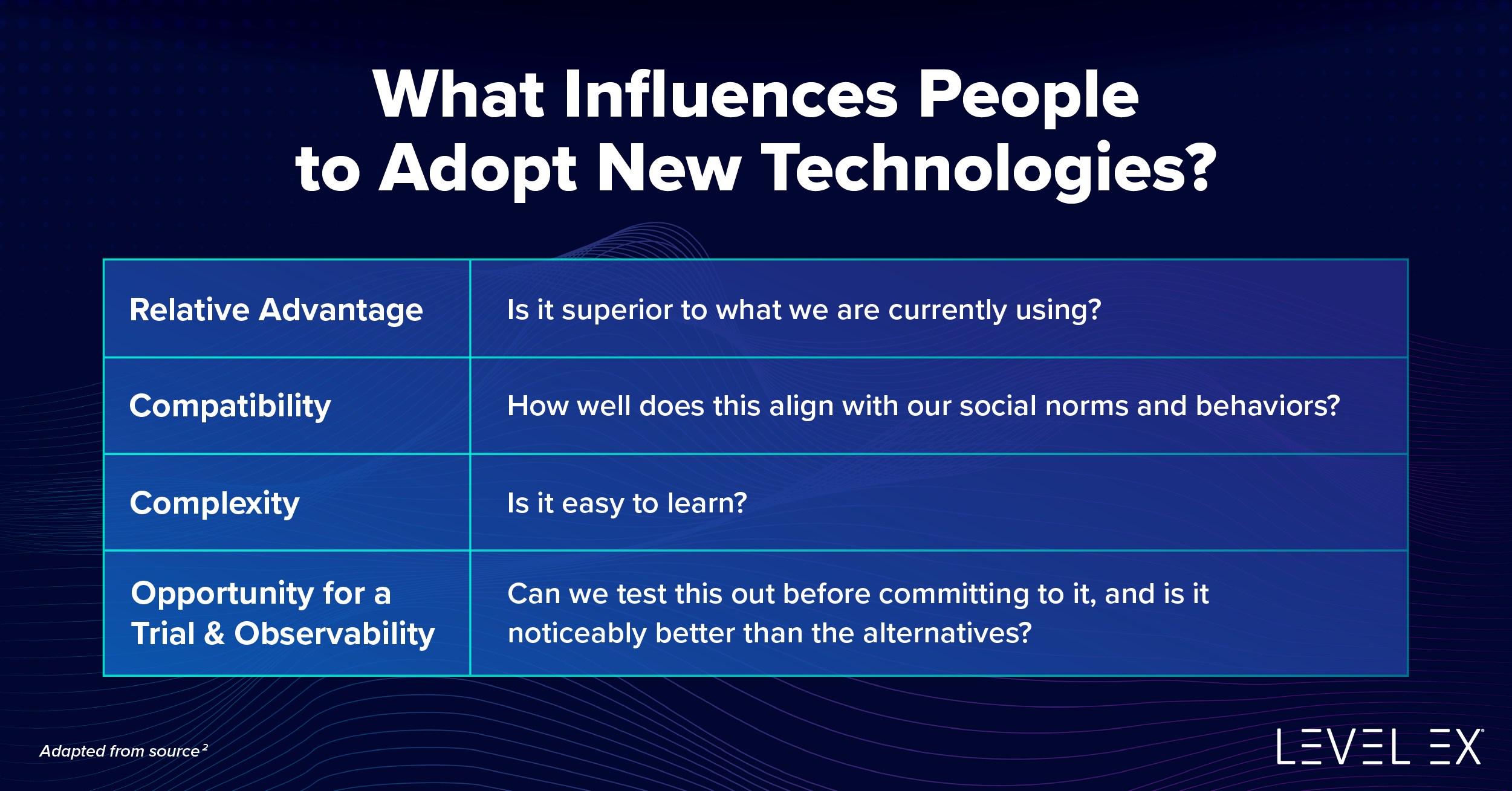
Dr. Gantwerker: I couldn’t have described that better. I’d like to borrow that. Taking a step back to give it some historical context, Level Ex was built on the idea that we can use the technology of games and the mechanics and psychology of games to create medically relevant content. Historically, we’ve done a lot of procedure-based games. We started introducing some medical decision-making games, critical thinking, and judgment. This is a new genre for us where we’re creating challenges and knowledge-based challenges of diagnosis, treatment, judgment, clinical decision making, and all the things that Peter and Michelle, we’re talking about—all in one game.
The best thing about it is there’s so much agency for the players. If you want to work on some adult dermatology, oncology, or pediatric dermatology, you can self-select the types of things that you’re in a mood for. If you want to do some quick hit binary sort, you can choose that. If you want to do some more deep thinking, you can do some more of the ”sticker situation” where you’re matching different things to decide the next steps.
This game was built to be whatever it is you want it to be. If you want it to be more fun and lightning, if you want to do stuff that has a little bit more challenge and may be harder that simulates some of the Boards type of stuff, you can. It’s there for you, and it’s your choice to do what you want with it.
Dr. Johnson: For any of our listeners who doubt that Peter Lio likes games, I know this is a podcast and you can’t see him, but I can. On the wall behind him is what seems to be a complete map of the original Legend of Zelda from the Nintendo entertainment system. Is that correct, Dr. Lio?
Dr. Lio: That is absolutely correct. Bravo. Not everybody knows what it is. Many people call attention to it and say, “Is that a microchip? What are we looking at?” But that is an eight-foot by four-foot, huge, beautifully printed fabric map of the original Legend of Zelda overworld.
Dr. Gantwerker: I don’t know if I’m more impressed that you have it or more impressed that he knew what it was.
Dr. Tarbox: I’m not surprised Luke has an epic level of nerdom that I have great respect for. Speaking of nerdom, I am a self-proclaimed dermoscopy nerd, and there is a dermoscopy game that is a part of Top Derm, and I really appreciated that. It’s teaching the three-point checklist, which is one of the more simple, usable formats for dermoscopy. I thought that the images were really good and that the feedback that you get after you play the round is really helpful. So super excited to see that.
Dr. Johnson: Do you want to ring our bell and tell us what the three-point checklist is?
Dr. Tarbox: I don’t have the bell. So this is a candle. [dings candle]
Dr. Johnson: Come on. We sent you two of them.
Dr. Tarbox: I had to switch offices at the last second because I changed my password in Microsoft and now I can’t remember what it is. So the three-point checklist. Ding. I’m so sorry about this. So it includes having an atypical network, having asymmetry, and having blue veil structures or blue-white veil structures—people describe this a little bit differently. A lesion gets one point for each one of those things. Any score of two or three is going to be more of a worrisome lesion. Three is very worrisome. Two is you probably need a biopsy. Normal lesions can have a score of one or zero. I thought that was a great way to reinforce that teaching and the way that you describe each little photograph underneath—very helpful. I also love the playfulness of some of the games. So there’s a rock and roll game that is hilarious and has had me singing “Come together right now” all day. So when are you guys going to explain that one?
Dr. Gantwerker: That was one more of my favorites. We like to have a little bit of fun when we’re creating these games. One of the creative opportunities that we have is the names and how we label things. That was one of the binary sorts that you’re trying to decide to either “Let It Be,” or I can’t even remember what the other option—
Dr. Tarbox: If it’s infectious, they’re supposed to “Get Back.” So that’s the Beatles song, [singing] “Get back to where you once belonged.” Then if they’re noninfectious, they can “Come Together.” So if it’s mycosis fungoides, they can come together and look for a medical treatment. If it’s herpes, then they can get back and not transfer it to other band members, which I thought was hilarious.
Dr. Gantwerker: There’s also another Beatles reference where there is a binary sort, whether you should biopsy or not. All I remember is if you don’t want to biopsy, it’s “Let It Be.” Peter, do you remember what the biopsy one is?
Dr. Johnson: It’s “Ticket to slice.”
Dr. Lio: Yes, that’s it. I love it.
Dr. Johnson: Listeners, I presume that you’re already convinced that you should check out this game. But I just want to give you an idea of what the experience is like. This might be incorrect, but the experience that I felt I had was like flashcards turned into a game show. I originally was going to say “flashcards made fun,” but we’re all nerds. Flashcards are already fun! There are these different categories. You have lots of pictures. I think every question that I looked at had a photograph associated with it. Then there are different versions. There is matching and then what you refer to as “binary sort”; you say “Let It Be” or “Come Together” and stuff like that. It has the feel of an old-school question bank, which I love, but in a much more fun way. It tracks your progress and lets you select different categories and different ways that you want to experience your education.
Dr. Tarbox: To me, it felt like You Don’t Know Jack, but for dermatology. If you ever played the game You Don’t Know Jack, there’s “dis or dat,” which is like the binary sort. Then there’s the matching and the questions. I just love it.
There are definitely little serotonin bells built in there to reinforce your learning. I always think that makes your brain work better, too. That’s why I’m very reinforcing when I teach my residents. You get little experience points, which I love. You have levels up and you unlock challenges. It’s very encouraging to move along and progress in the game, which is super fun.
Dr. Gantwerker: You hit on something important and that’s the strong tie between emotion and memory. We know things that are activating are always going to be stronger in your memory, whether it be negative or positive, which is why people always think pimping actually works. Pimping does work because you’re activating them, but you’re activating them in the negative zone. Games try to activate you in the positive zone. And that’s why Sam, our CEO, used to always say that your kids remember a hundred Pokemon characters, but not 40 US presidents. That has to do with the emotion—that strong tie between emotion and memory.
Dr. Johnson: Again, if everybody is convinced that they should go out and check out this game, since we’ve got medical education experts, I’d like to discuss topics relevant to that. How can our listeners who are interested in learning more, or who are educators themselves, leverage what you guys know, that we might not, to help teach both themselves and their learners?
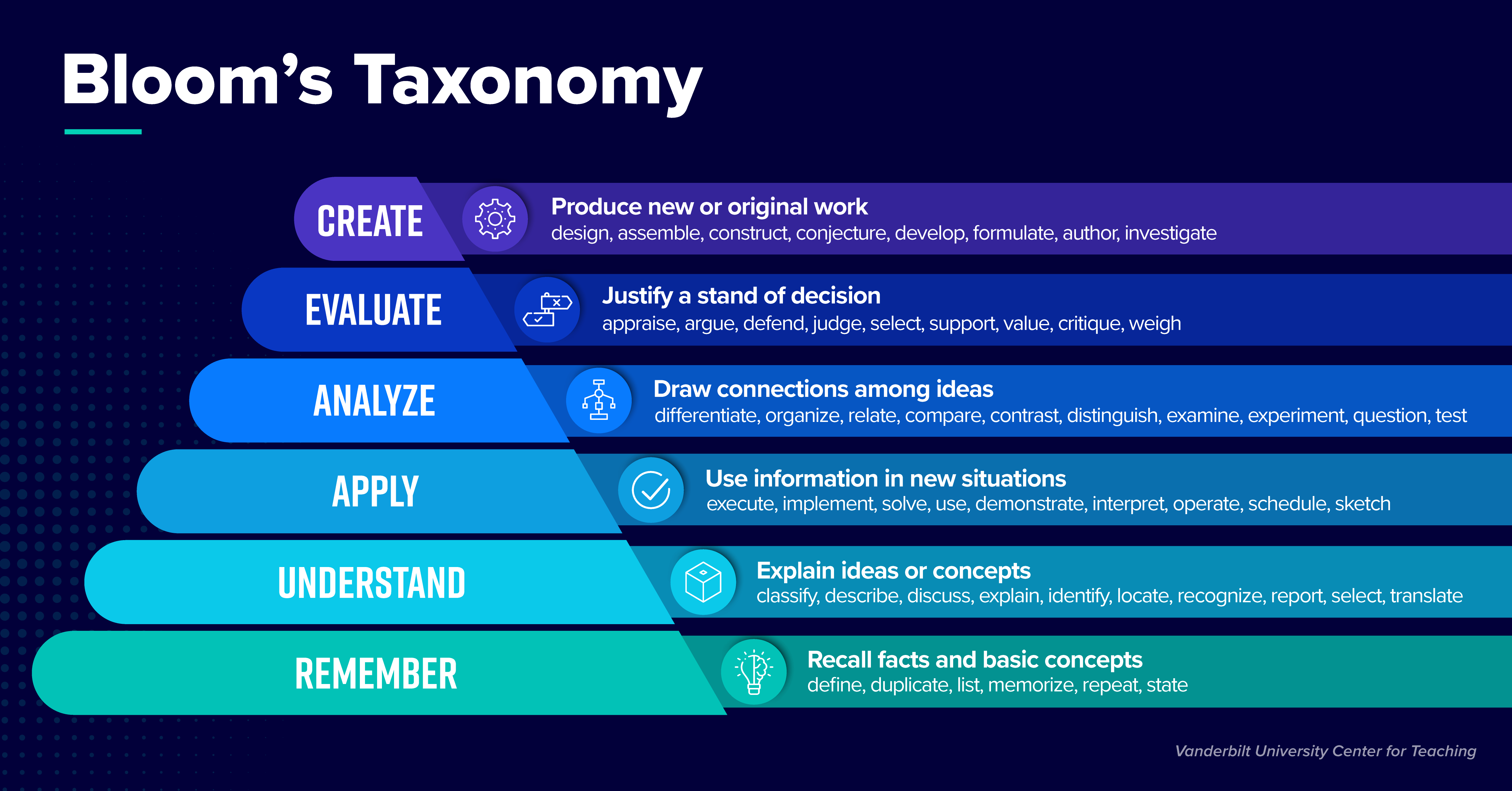
Dr. Gantwerker: I’ll say that you all might be dermatology nerds, but I’m a cognitive science of learning nerd. If that doesn’t come across, I’ll tell you upfront that that’s my bag. I’m interested in motivational theory and in what motivates people. One of the things that attracted me to games as a learning platform was the fact that games are an opt-in experience. You are intrinsically motivated to play games. The way the games create environments in which you are intrinsically motivated to not only start the game but persist through challenges. I’m sure there were very many challenges in Legend of Zelda where you were ready to give up, so how do games create this motivational pattern to have you persist through challenges?
The way that medicine is trying to teach our future clinicians of tomorrow is we’re trying to teach them to face challenges. We’re trying to teach them to problem-solve. We’re trying to teach them all the different ways and patterns of things and how they can be presented in a clinical environment and understand those patterns and make decisions and judgments. That’s literally what games do in an intrinsically motivated pattern. It was so exciting for me when I started working for Level Ex back in 2016. It’s been solidified for me that games are the right way to do this.
Dr. Tarbox: One of the great things, too, that I found exciting about the app is that you’re touching on neglected areas of dermatology. There’s a focus on the treatment of patients who are pregnant and medications that are appropriate or not. There are lots of images of skin of color, which I think is very important for us to be able to provide complete healthcare to all of the patients that we take care of. Then there are operational guidelines that we need to have cold as dermatologists, but those things are just so hard to learn by rote. There’s a really fun game that’s helping you understand the NCCN Guidelines for squamous cell carcinoma and which treatment is appropriate for what? Which one’s a high-risk lesion? These are all things that will help people to practice more efficiently and also more effectively.
Dr. Lio: It’s so true, you know, I’m a medical derm almost exclusively, and about half my practice is pediatric. Early on in the discussion a couple of years ago, we were saying, “What’s easy and what’s hard?” I learned quickly that that depends on your point of view. If you are mostly doing Mohs surgery, then even some basic pediatric dermatology is not so basic. It’s like, “I don’t really see kids anymore.” We tried to get a gradient for each of these things so that people can dabble. We don’t want you to go in and be like, “Oh my gosh, it’s all crazy genodermatoses that are super rare, and I don’t want to do this anymore.” We want to have some easier stuff. People say, “Oh, yeah, I remember this. OK, right.” Then they can build up and strengthen.
I love that you brought up, Michelle, the idea of strengthening your own. We have that radar plot, that spider chart, where you can strengthen on all those different forms to become a well-rounded “Top Derm,” if you wish. Maybe you’ll just pick your own area to just practice and kind of test your might, or maybe you’ll pick your weak point and say, “I just want to spend time just focusing on this area.” I love that there’s all that flexibility and again, potentially for the future, to even add more modules and more new experiences, because this is a great way to learn. I don’t love reading journals anymore. Right now, we have all these other awesome ways to do things. So journals can be the springboard, but this is a way to really bring it to life.
Dr. Johnson: Podcasts. Another good example.
Dr. Tarbox: Exactly. One other thing I want to clarify, just if anybody who’s listening has any questions about this. Sometimes whenever a computer is involved and decisions are being made, people get concerned, in the days of artificial intelligence (AI), that we’re training our replacement overlords of robots. There’s no way this game could do that because this is not using us to say, “Is this bad?” It’s telling us, “You said this about this lesion, and this is what’s correct.” So the game already knows. We’re not teaching it anything it doesn’t know. This is not us training our robot overlords. It is us making our brains, which are a little computer-like, kind of a mushy biological computer, work better. I think that’s amazing. If anybody’s concerned about that, you can allow yourself to take a deep breath and realize that you are just making yourself better. You’re not helping out the AI.
Dr. Lio: Yes, I know people were kind of nervous. Whenever they see sorting, it’s like, “Are we training it?” But here, these are all known quantities. They’re all hand-done now. The computer didn’t organize them. These are all hand-done by humans. So the right answer is what we put in. Now, of course, there may be mistakes. In that case, we want our users to say, “Hey I’m flagging this. You’re wrong on this,” because this is truly hand done. The AI discussion is interesting. It just, fortunately, does not apply to this setup right now in any way, shape, or form.
Dr. Gantwerker: Peter hit on it. Something interesting in this game that’s different from our other games is the ability of players to give us feedback. Oftentimes when people are playing our games and they want to give us feedback, they send us an email or go to our website. This is feedback integrated into the game because we want to hear from people to say, “Hey, this is what I want to do. This is what I’m interested in. This is what I’m motivated to do.” Having that explicit communication with our player base is something completely new in Top Derm that I’m excited about.
Dr. Tarbox: I saw that feedback button right at the bottom of every game. After you’re done playing, you can leave feedback for any question that you have. You could leave like, “Hey, great job.” Or you could say, “I think this question might be better written this way.”
The images are amazing, so I’m glad you brought up the tuning of the images because I was like, “Oh, wow,” because there was a port-wine stain, and I was like, “That is the port-wine-iest port wine stain that I have ever seen.” This is just a good way to sort of imprint the chief characteristics of what you’re looking for. It’s almost like how Netter images are the way that we learn basic anatomy when we’re going through medical school, because the structures are hyper-real in a way, in that they can be more classified into the boundaries of the lesion and the defining characteristics. It’s just easier to learn that way. I used to make dermatopathology cartoons for the same reason.
Dr. Gantwerker: It’s really interesting because all those images were peer-reviewed by Peter Lio and all of our dermatology advisors. Some of them were completely fooled as to whether they were real or not. You point out that some of them are hyper-realistic where it’s the quintessential picture of what that is, but the good news about our ability to create these images is that we can make them less discerning. We can make them more ambiguous. We can make them however we want. That’s the power. What Peter really believed in was our ability to create these images of any disease on any skin type and be able to create those so that it’s challenging. It’s interesting. We don’t have to rely on the images that exist out in the ecosystem, which we know aren’t representative of all the diseases we see, especially in skin color, like you brought up earlier.
Dr. Tarbox: I love the atypical locations, too. Like the bullous lesions, which were almost always shown on trunks. They were on acral surfaces, so you have to think about them a little bit differently. They teach you the right way to do the proper biopsy, which as a dermatopathologist, I absolutely love. I was like, “Yes, scream it to the mountains.” That was very nice to see.
Dr. Johnson: This is fascinating. Let me make sure I understand: The photographs that we see in the game are not just “somebody took a picture and uploaded it.” They’re somehow modified by graphic artists?
Dr. Gantwerker: We have a mixture. We have ones that we’ve sourced from either dermatologists or atlases. We have some that we’ve gotten through partnerships. Then we have the ones we create. The ones that we create are in instances where there aren’t a lot of good examples or there’s something we don’t have really good examples of this skin condition on this location, on this skin type. If they don’t exist, then we’ll create them.
That’s one of the hardest things and why I’m so proud of our team. They’re making images that don’t have reference images. Just think about creating something, drawing something, that never had anything for you to reference, and you’re not medical, so you don’t know what you’re even looking at. That’s where our advisors come in. That’s where Peter Lio has been invaluable in this, and all of our derm advisors, to say, “You know what? I’d make it a little bit redder. You know, subsurface scattering is a little bit different. The lighting is a little bit different. I would extend this a little bit.” That’s where it comes to life.
Dr. Lio: It was so cool because they’re rendering the skin in this sophisticated way. It has depth, moisture, and all these different qualities. It’s not just a sketch. Sometimes they would show me an image and I’d be like, “Ah! I don’t know! Something’s wrong about this. It feels too dry or it feels like the texture is wrong.” You’re trying to explain it to the artist. It was so cool. They understood that language, too. It was just uncanny. You’re like, “What you’ve just shown me is really wild. It looks good, but this doesn’t exist. This is wrong.” Then they’d spend a day or two, and you would get this new image like, “Yes, that’s right. That feels correct. That looks right.” It was a whole new level of language processing for what we’re seeing because they can defy the laws of biology. They can make whatever they want. They can make a wet lesion in the context of dry scale or something crazy like, “Whoa, this shouldn’t exist.” It was so fun to fine-tune that. I think that’s something that’s going to keep happening. It allows us to paint a particular situation for any kind of clinical scenario we want to bring up.
Dr. Tarbox: That’s really cool.
Dr. Johnson: That’s really innovative. Now there are two innovative things about this. There’s the gamification. Plus there’s this very fascinating graphic art rendering of dermatologic disease. As somebody who is a dermatologist and would use the game, I could be assured that even though the image was created rather than actually photographed on a patient, I can trust that that’s what it would really look like in person because smart dermatologists like Peter Lio have agreed that that’s what it should look like. Is that fair?
Dr. Tarbox: And actually give the feedback to shape, it sounds like?
Dr. Gantwerker: Yeah. They worked literally side by side, as Peter Lio talked about. We do have a lot of images that are photographs taken by dermatologists or that are available that we sourced as well. It’s not all computer-generated. We source it. We focus on the computer generation of things that there aren’t a lot of reference images for. Everything else—the typical atopic dermatitis, the typical acne, all those types of things—is usually available. It’s the hard-to-find ones that we’re trying to focus on.
Dr. Tarbox: Well, there are some things that I feel like we all were trained on the same five images of—
Dr. Gantwerker: We always saw the same Wartenberg picture as an ENT. Every single one knows that one kid with Wartenberg’s.
Dr. Tarbox: Everyone knows the young lady that had chickenpox. We all trained on that one picture of that one young lady with chickenpox. It’s just like, “Wow, you’ve seen it once!” I think that having the ability to diversify that and build our visual library is very beneficial. We were talking about the AI bots, but that kind of learning is based on the way humans learn. Every time we see an image and we understand and know what it is, we add to our own visual library, and that increases our sophistication as we diagnose and treat patients. That’s awesome.
Dr. Gantwerker: Yeah. And that strong imprinting of how you learned changes the way that you practice. If you only saw chickenpox on somebody who was fair-skinned, Fitzpatrick skin type 1, then seeing chickenpox and somebody who’s a different Fitzpatrick skin type is going to be very difficult for you. One of the things we’ve tried to focus on with this technology is creating those images so we can change your imprinting.
Dr. Tarbox: It’s awesome.
Dr. Johnson: So we mentioned this AI thing. I think another aspect that people might have a question about is if this game doesn’t cost anything to download, then how do you guys keep remaining a business?
Dr. Gantwerker: I work really hard. No, just kidding. When Sam and everybody created the company, the goal was to democratize this type of content and use games for good and for a purpose to try and bring everybody up to the same level within their specialties. In that, he wants to democratize it and give access to everybody. He always wanted it to be free. He didn’t want to have doctors or institutions pay for it. He wanted to have access, which is why it’s mobile.
The way that we monetize is similar to any other free platform. We work with societies and organizations. We do some grant work, and we work with industry partners and clients to help get content that is specific to them or trying to work on specific challenges that would be applicable.
The example I always give is in our anesthesia game, Airway Ex; we worked with the American Society of Anesthesiology. They were very specific about some of the needs that they were seeing based on malpractice insurance claims showing that doctors weren’t getting the difficult airway algorithm. We recreated the difficult airway algorithm within our game and helped them to solve some of the problems that they were having in a creative way. I think that’s the way that I look at it. We work with these partners and clients to solve problems in a creative way that otherwise didn’t have good solutions.
Dr. Tarbox: One of the amazing things about democratizing education is that you’re not just elevating the state of practice of the physicians that play the game, you’re elevating the state of healthcare of the patients they take care of. That helps improve the entire quality of healthcare across our very diverse and very unique country. And so it’s really a noble mission. I’m very impressed by that.
Dr. Johnson: Dr. Gantwerker, you just alluded to this, but Top Derm is not the only game that Level Ex makes. Some of our listeners might be or know people who practice in other fields. What else do you have out there?
Dr. Gantwerker: Top Derm is our fifth title. Our first title was Airway Ex. After that, we had Gastro Ex, Pulm Ex, and then Cardio Ex. So we have four different specialties: anesthesia, cardiology, gastroenterology, and pulmonology. Top Derm is our fifth and newest title, but we continue to try and change the way the different specialties can consume content. Dermatology we’re very excited to be working on next.
Dr. Johnson: How come it’s not called Derm Ex?
Dr. Gantwerker: That is a great question, I think Peter had a small hand in this as well. There are a lot of things that we were thinking about, and we talked to our dermatology advisors and felt that Derm Ex didn’t capture what we’re trying to do. I don’t know if Peter has any comments on it either.
Dr. Lio: The underpinning for pushing this forward is to make you better. In the back of our mind, the goal we’re going towards is by doing this game, by playing and practicing, you’re going to be able to become a “Top Derm.” That was the concept. We really liked it. I thought it was unique and different and also gave us a little bit of a new space to start thinking about. Like when Apple switched from “i” everything to switching things out.
Dr. Gantwerker: We also didn’t want people to think that this was some kind of medical therapy. Right? Derm Ex, you know, get over the counter for your psoriasis, but—
Dr. Tarbox: It sounds like a medicine. That’s what I was going to say. It kind of sounds like it could be a drug.
Speaking of drugs, I did notice that you’re using the generic names. For any educational purists in the sphere, it is absolutely fine to recommend this for resident use. It teaches really important points about those medications that our residents need to be familiar with, like if it’s appropriate to use in the state of pregnancy or something like that. I thought that that was a lovely point to emphasize so that people feel comfortable.
Dr. Gantwerker: Absolutely. To build on that, all of our games have CME. CME content is coming to Top Derm. Not only do we believe that we should use generics and keep it unbiased, but we also have to for CME purposes. Any of our sponsored content has to live separately from our CME content, so we just by principle do that. That’s one of the things that we strongly believe in.
Dr. Johnson: Again, I want to dip into your unique expertise as technological innovators and medical education experts. Where do you project the future of medical education to be and how it combines with technology, not just in games and excellent podcasts, but over the next 10 to 20 years?
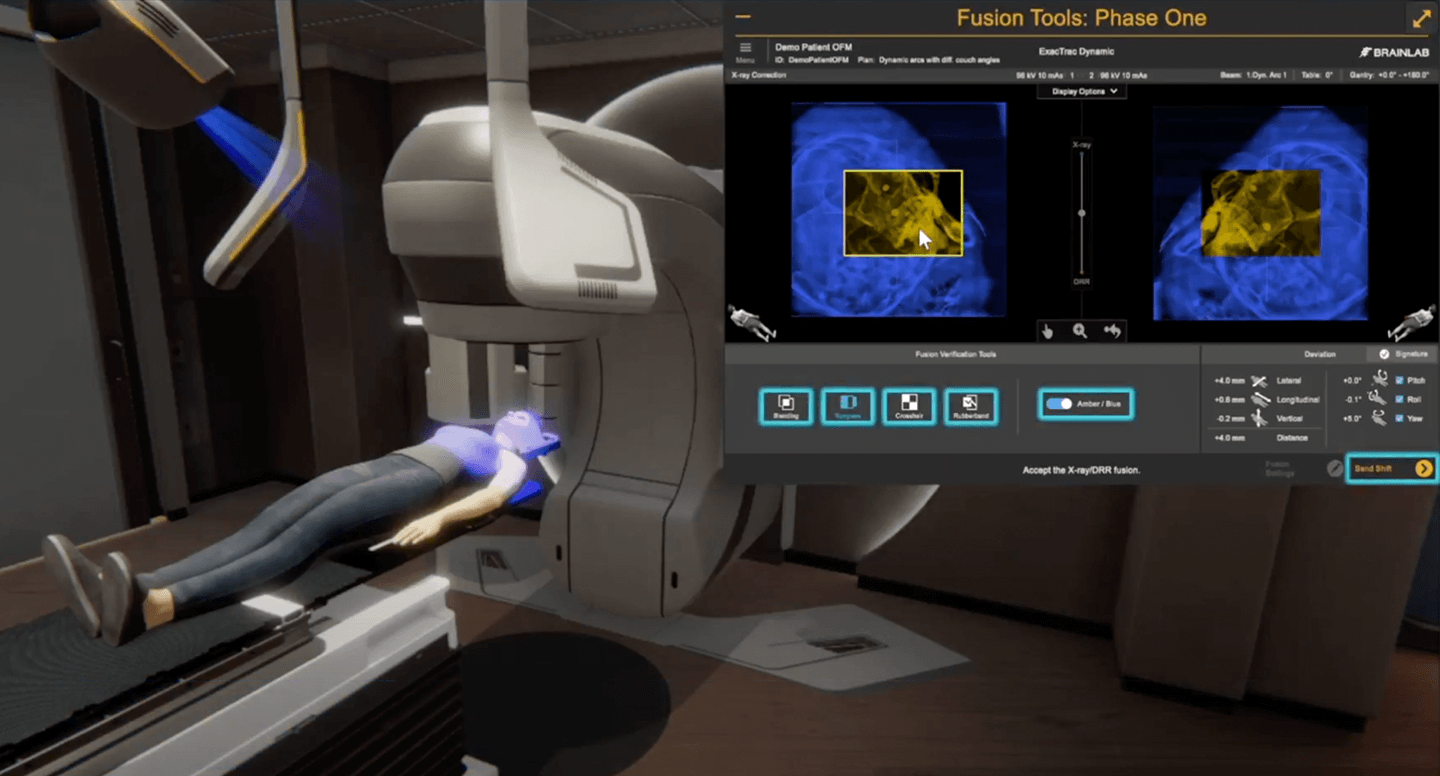
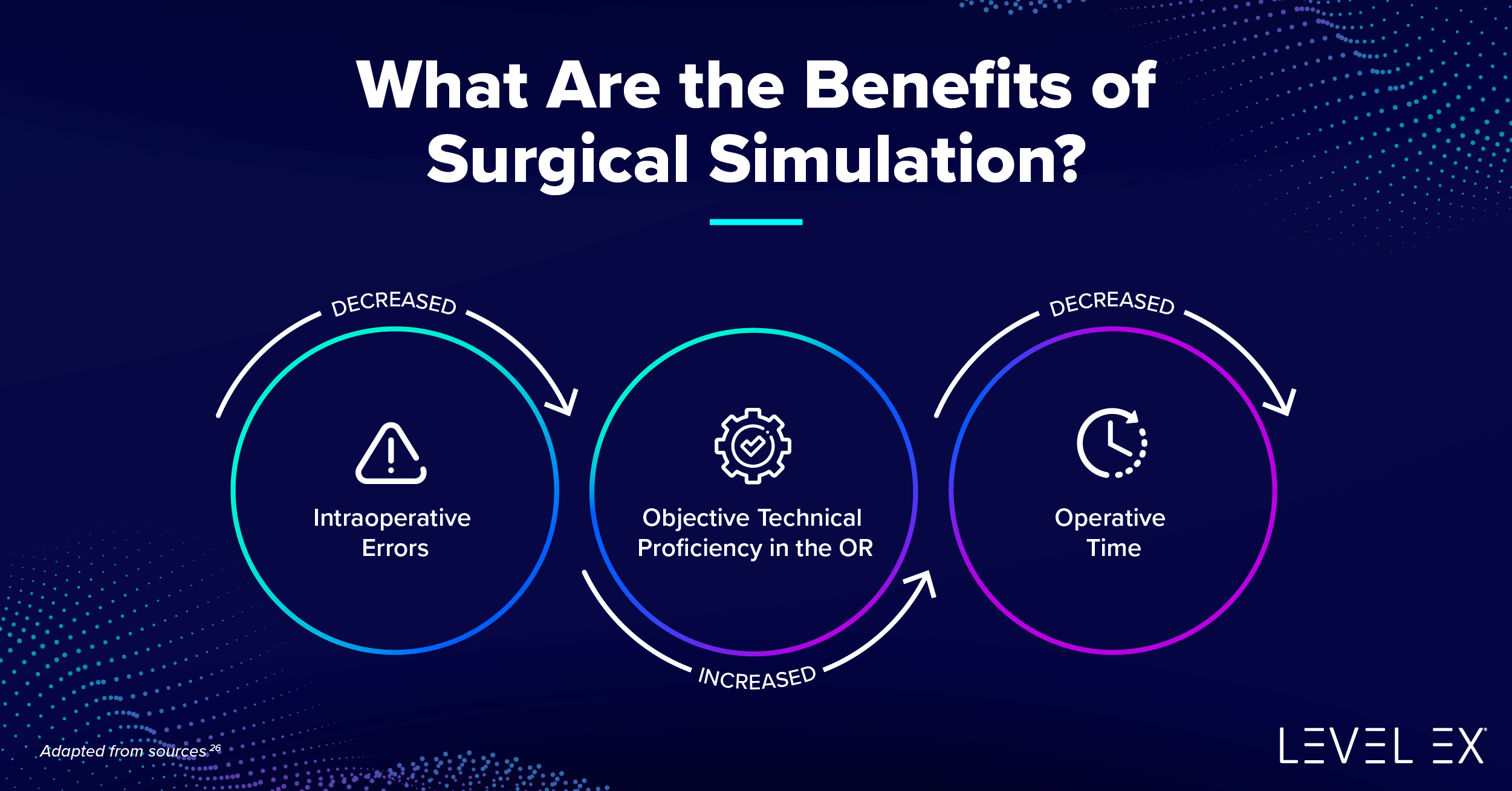
Dr. Lio: The future is podcasting. I’m pretty sure you guys are the tip of the spear. I do think that with improved technology, we’re going to see the sim movement. Simulation is such an important part of medicine. It has been for a long time, but it is, so far, synonymous with big clunky mannequins and getting up at five o’clock in the morning to do a surgical trauma sim with everybody in the room. It’s pretty cumbersome, although I think there are some amazing outcome changes.
What if we could bring some concepts and learning down, distill them into your mobile app, or, who knows, maybe in the next couple of years we’re going to have augmented reality and virtual reality that everyone will be having with them all the time? That’s my guiding light. If we can bring some of these same principles to everybody, we are going to see the best education in the history of medical education.
We come from a generation—all of us are old enough before there were work hours—so we put in a lot more time. As we cut down on that for our younger learners, and even for us, you can’t see everything in a given amount of time, no matter how good your training is. So we can augment and expand upon that in a way that will change everything.
Dr. Gantwerker: Building on that, you’re never going to come out of medical school or any kind of training knowing everything you need to know. We need to focus on teaching people how to learn. The doubling time of medical information is 73 days. The entire corpus of medical education is doubling—medical content is doubling—every 73 days. But, we take advantage of technology and how technology has advanced.
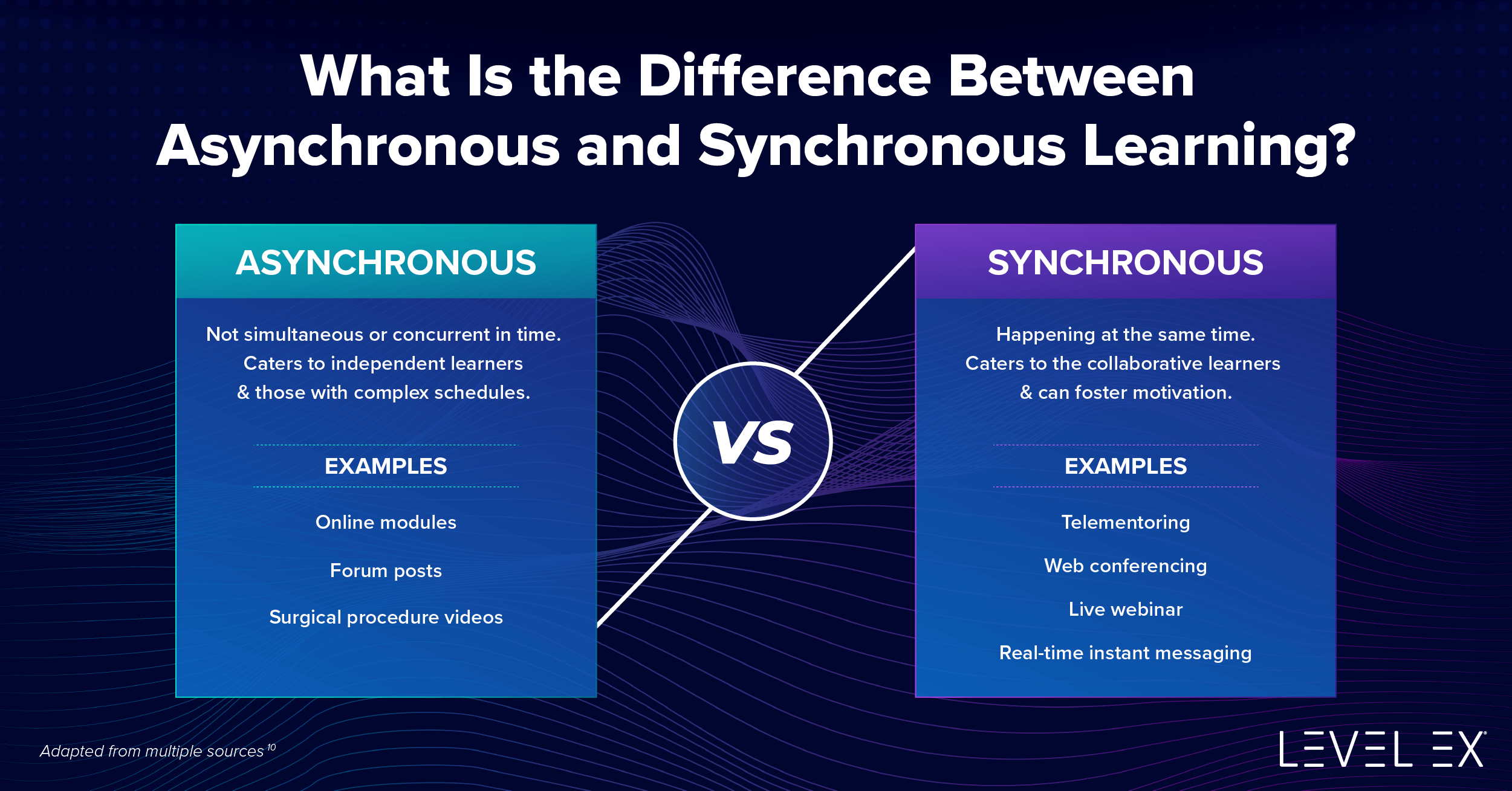
Simulation has been a great area for medical education. The problem is, as Peter told you, a lot of hardware-based solutions were always destined to have a problem. When COVID-19 hit, it shone a bright light on the fact that now these hardware simulations that are hundreds of thousands of dollars are locked behind doors, and nobody had access to it. One of the things that we saw explode was asynchronous learning. We saw synchronous remote learning and synchronous in-person learning diminish. And I think the future is: how do we leverage asynchronous learning and synchronous remote learning and then save synchronous in-person learning only when necessary. Software-based simulation and software-based solutions are going to be the answer.
Dr. Johnson: I also think that AI is going to play a big role. I know we touched on that briefly. My personal feeling is that it’s not going to replace us. It is going to assist us in some ways with decision support. So, for example, if you take a dermoscopic image, the computer might say, “Hey, this has a blue-white veil and an atypical pigment network, that’s two points, dummy. Maybe you should biopsy it.” But also people will be able to take pictures of stuff on their phones and they’re going to come in and see us for stuff that their phones don’t have a good answer to. It’s going to be like the equivocal lesions and then it’s going to be our job to figure it out. Those are the hard things that we do. So, I see that kind of thing coming too, even though maybe it’s not directly related to medical education.
Dr. Lio: I really like that. I like that so much because sometimes people will say, “Oh, derm, you guys are doomed because everything you do is just diagnostic and the computer is going to do it.” But it’s like, “Really?” The diagnosis for 90% of my patients or more happens in the first 10 seconds, or even when they walk down the hall. I know what they’re here for. Sometimes it’s in the current complaint. If the computer can take that over, OK, that doesn’t affect us too much.
I think you’re totally right—that decision support and augmentation of knowledge. What’s the current best therapy for when a patient fails something? You can read the textbook and the evidence tells you maybe one, maybe two. What if they fail both? Now what? It’d be cool to have a little decision support that says, “OK, well, there’s a little bit of literature here. This might help us here in this context.” Especially as we get towards more personalized medicine, which is my goal—to look at a patient and to understand specifically what is their genetic background and what is their phenotypic background. We can customize a treatment protocol for them that not only is the best therapy for them, but also has the least side effects.
We’re learning about this right now with some of the new medicines. My area is atopic derm, and we’re seeing scenarios like, “Whoa, this side effect only happens in one group of people. What if we could figure out who that is and exclude them?” We might be able to use the medicine a lot more safely, but this is going to become an exponential amount of data. I think we’re going to need peripheral brains to help us digest all this and bring it up to the forefront.
Dr. Gantwerker: Absolutely. Radiology was probably the first area that felt threatened by AI. Bertalan Mesko is a medical futurist who said that radiologists who use AI will replace those who don’t. It’s the idea that resisting it is futile. No, I’m just kidding. Resisting the ability to focus on what you can do as a clinician: the medical decision making, the judgment, and the amount that we can do with the external brain. Again, with the 73 days turnover time for doubling of medical content, you as a clinician can never know everything that’s out there. Why not offload that onto a computer? You already do. We Google things all the time. We look things up. We’re always using computers, imagining. Twenty years ago if they said: “You can be a doctor, but we don’t want you to use the Internet.” How would you have responded then? This is the new evolution, the new industrial revolution, of bringing AI into all aspects of our lives.
Dr. Johnson: As long as we’re off on this digression, something else that I think might be important in the future is more computer modeling. I remember being a medical student, and I was kind of offended when I discovered that the placebo-controlled, randomized trial was the gold standard. “Why do we need to spend millions of dollars and get five thousand people to figure this out? Can’t we, like, draw blood on a bunch of people and chug it through some fancy computer system to measure six hundred different micromolecules and then see what happens to different people when they take particular medicines?” My hope is that something like that can come as well.
Dr. Gantwerker: I think there’s a lot of opportunity in big data. We had talked with a company that is using CT scan images of lungs to predict best ventilation plans for patients in the ICU. They use the big data from all the CT scans of the chest of patients with different diseases. They could create a computer model that can tell clinicians at the front end, “Based on this patient’s CT scan, this is the recommended ventilation that’s going to be best and most optimal and best survival for this patient.” Why would you not want to be able to use that type of technology?
Dr. Johnson: Especially if I was reallocated to some kind of COVID-19 unit.
Dr. Lio: Definitely.
Dr. Gantwerker: Absolutely.
Dr. Johnson: Well, guys, as we wrap up here since Top Derm is kind of like a game show, I want to give the two of you some game-show style questions.
Dr. Gantwerker: Do we have a theme song? Yes, that was it.
Dr. Johnson: I’m going to start with fill in the blank. You can each answer. So “The thing that I am most proud of about Top Derm is blank.”
Dr. Lio: For me, it’s that it is accessible to learners of a huge range. It’s not just designed for somebody who’s an expert in one particular field. Lots of people from many different specialties, potentially, could play around and learn some basic dermatology from it.
Dr. Gantwerker: I will say I’m most proud of our team for bringing so many different elements of games into a totally new genre for us and using these computer-generated graphics, which is, I think, groundbreaking. If anybody looks at them, they’ll realize the power that this technology has. But using those game technologies, using those designs to create a really one-of-a-kind type of experience.
Dr. Johnson: All right, good answers. One more fill-in-the-blank. “In terms of the future of technology and medical education, maybe we already discussed this, I am most excited about blank.”
Dr. Lio: I’m most excited about personalized medicine coming in, as you described beautifully, where we’re going to be able to instead of doing randomized controlled trials, we’re going to be able to give a specific patient, with the power of technology, exactly what they need, just in time. That’s going to change. It’s going to change everything for the better.
Dr. Gantwerker: I’m most excited about the power of adaptive learning and dynamic content-serving—the idea that you can train during your medical education residency on the things that you need to train on instead of just saying, “You need to be here for four years, and whatever we can teach you in those four years is what you get.” Whereas, “We want you to be the best thing we can be in four years.” Trying to say, “You know what, you’re really good at dermatopathology, but you’re really bad at this. Let’s focus more time on this.” Once we do more adaptive learning and really specific personalized learning experiences, I think we’re going to make much better clinicians.
Dr. Johnson: I, as a parent of young children, would also be excited about that stuff for my young children. So here’s to hoping that that comes around while they’re still in school. All right. Two more questions for you guys. Both multiple-choice: most physically attractive Dermasphere co-host is A, Luke, B, Michelle, or C, all of the above.
Dr. Tarbox: The pimping bell, which I don’t have. It’s gorgeous. You’re going to have to take my word for it.
Dr. Gantwerker: Can I get a write-in for the Legend of Zelda map? That’s really the—
Dr. Johnson: Man. I lost the attractiveness contest to Legend of Zelda map? There’s a first time for everything. OK, finally, the funniest Dermasphere co-host is A, Luke, or B, all of the above. I’ll just let listeners make their own judgments on that one. As a reminder, you can write notes in the margins of your test, but they won’t count for scoring purposes.
Dr. Gantwerker and Dr. Lio, thanks again so much for being here and for making this cool game. So tell us where people can find out more about it, more about Level Ex, Twitter handles, and other social media, so we can put it in the show notes.
Dr. Gantwerker: For sure. They can find us on the interweb at www.levelex.com. You can find us on Twitter @LevelEx. We’re also on LinkedIn as Level Ex Inc. They can also find me @DrEricGant on Twitter and Eric Gantwerker on LinkedIn.
Dr. Lio: I’m most active on our Twitter, which is @ChiEczema, for the Chicago Integrative Eczema Center. And then that’s also our website: ChicagoEczema.com.
Dr. Johnson: Perfect, we’ll put those in the notes, guys.
Dr. Gantwerker: You can download all of our content for free in the App Store and Google Play. You can find Top Derm under that, as well as links to our Airway Ex, Gastro Ex, Pulm Ex, and Cardio Ex games.
Dr. Johnson: And listeners, thanks to you guys for joining us today. If you are new to Dermasphere, welcome aboard. Happy to have you. If you want to keep riding the Dermasphere train, here are good cars you can head out to keep it rolling. So of course, episode 47 with Peter Lio. Our two most popular episodes are episode 44 (we talk about over-the-counter hair supplements, among other things) and episode 49. We talk about environmental causes of skin aging, among other things. So a lot of people like those.
If you’re new to us, you might want to check those out. A nice Dermasphere sampler is a recent bonus episode that we put out called Pearls Floating in the Dermasphere, where we touch on some of the highlights from our first two years. Dr. Lio and Dr. Gantwerker, any final comments before we bid you adieu for now?
Dr. Lio: Thank you so much for having us. It’s so much fun, and I can’t wait to hear the next episode of Dermasphere.
Dr. Gantwerker: Yes, and I thank you again on behalf of myself and Level Ex. We really appreciate it and we’re super excited about this game. Thank you so much for having us on.
Dr. Johnson: We are excited as well. And listeners, you know where to find it. If you would like to find more Dermasphere here, you can find every episode, including the topics we cover on each on our website, DermaspherePodcast.com. You can also find our entire archive on Apple podcast or wherever you get your podcasts. And you can find us on social media, too. We are on Twitter, Facebook, and Instagram. That’s the other one. I’m too old. Thanks to young person, Ryan Carlisle, a medical student and member of our team who keeps those moving along. We will see you guys next time for our regularly scheduled stuff.
Thank you to Dermasphere co-hosts Michelle Tarbox and Luke Johnson for having us on the show. If you enjoyed listening, you’ll love playing. Download Top Derm now.















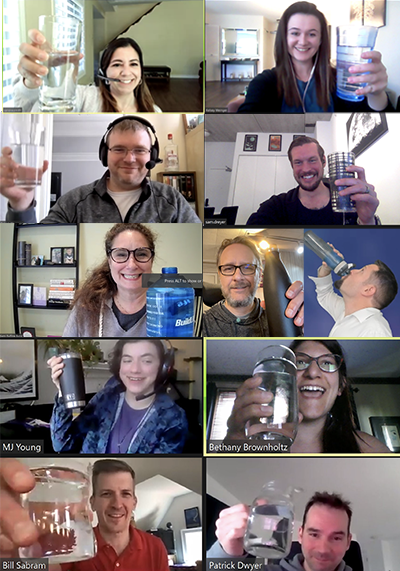 Cheers to hydration! Level Ex’ers started each meeting by raising a glass of H20 during the “Wellness Water Challenge.”
Cheers to hydration! Level Ex’ers started each meeting by raising a glass of H20 during the “Wellness Water Challenge.” 
 Studies show that employees who see nature from their office spaces like their jobs more, enjoy better health, and report greater life satisfaction. Level Ex’ers wear green to remind one another of the color’s positive effects on mental health.
Studies show that employees who see nature from their office spaces like their jobs more, enjoy better health, and report greater life satisfaction. Level Ex’ers wear green to remind one another of the color’s positive effects on mental health.

